This site contains affiliate links. I may earn a small commission, at no extra cost to you.
If you want to clear your skin and treat acne, you have to know what’s causing your breakouts. Just applying products or changing random things about your lifestyle likely won’t get you to your goal.
Before you do anything, find out what type of acne you’re dealing with. There’s regular acne, fungal acne, hormonal acne, comedonal acne and even mechanical acne. I talk a bit about the different kinds in my post, “When to See a Dermatologist for Acne.”

If you have polycystic ovary syndrome (PCOS), a common endocrine disorder in women, your acne is hormonal. But how is that any different from regular acne?
In this post, I’ll talk about these two common acne types, how they differ, and how you can treat them.
PCOS acne vs. regular acne: know the difference

Acne comes from both internal and external sources. That’s why you can’t fix everything with a skincare product that says “for clear skin.” It’s just not that simple. And in terms of PCOS acne (or, hormonal), oftentimes it takes healing both inside and out.
Learning about your acne type and its root causes is the best thing you can do. Let’s get into the difference between PCOS hormonal acne and regular acne.
What is PCOS acne?
PCOS is a condition that impacts a woman’s hormones. The hormonal imbalances, such as high testosterone, trigger a long list of chronic symptoms.
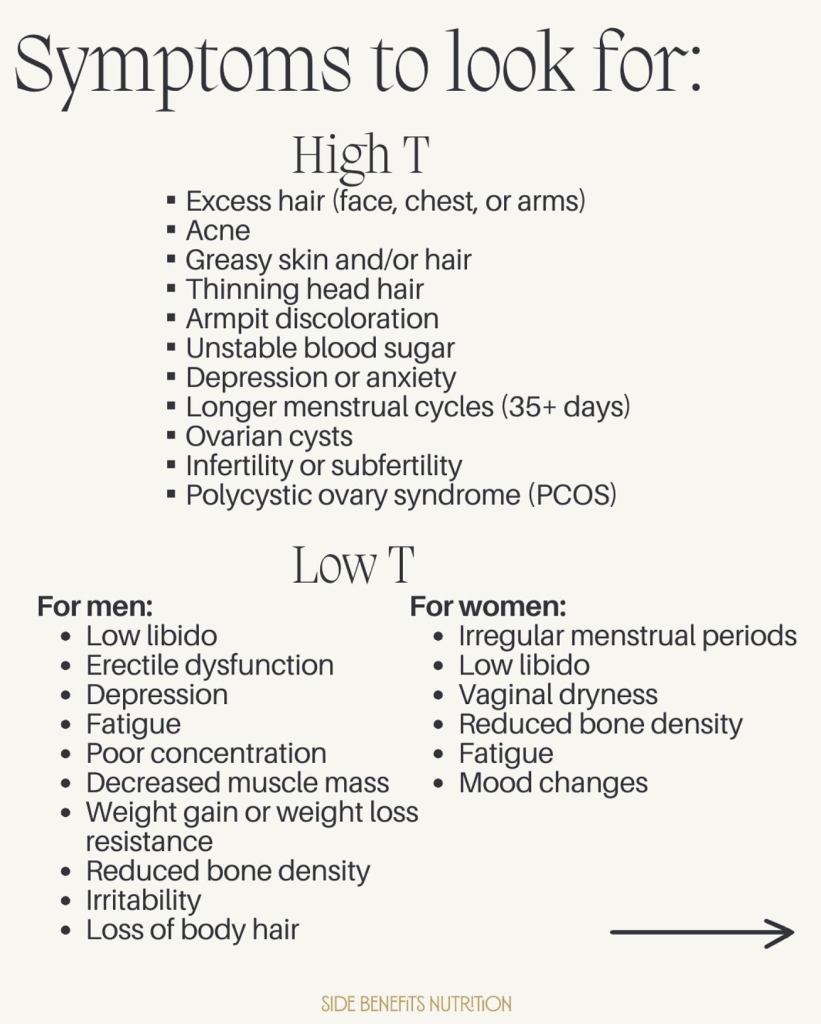
Hair loss, irregular menstrual cycles, excess facial hair growth, weight gain, fertility issues, mood swings, and yes, hormonal acne, are all rooted in high testosterone levels and insulin resistance.
So, though external factors like bacteria could play a role in acne with PCOS, the bigger problem is with the imbalanced hormones.
What does PCOS acne look like?
- Deep, cystic pimples that are painful to touch
- Concentrated along the jawline, chin, and neck (U-zone)
- Can extend to the lower cheeks and sometimes chest or back
- Fewer blackheads/whiteheads, more inflamed lesions
- Often worsens before a period or during hormonal shifts
- Leaves dark marks and scars more easily
What triggers PCOS acne?
Like a lot of chronic health issues, PCOS creates a cyclical problem that makes acne really hard to get rid of. Without the right management strategy, PCOS acne just spirals from bad to worse.
This is what happens:
1. Insulin resistance raises testosterone levels
Most women with PCOS have insulin resistance. This is when your body stops properly processing sugar, leaving it in the bloodstream and storing the excess as fat.
The high insulin levels prompt the ovaries to produce more androgens like testosterone. These high androgen levels throw other hormones off balance, as well.
2. Elevated testosterone increases oil production
Testosterone binds to receptors in sebaceous glands, which increases oil production overall.
The excess oil then gets into your hair follicles, blocking pores. When your pores are clogged, you get breakouts. Plus, sebum is the perfect ‘food’ for C acne bacteria in the pore who eat the sebum, and then cause inflammation within the pore. This is how inflamed pimples come to be.
If you frequently deal with this issue, you may enjoy my posts, “Skincare for clogged pores” and “How to Get Rid of Clogged Pores (and Four Mistakes to Avoid!).”
3. Suboptimal circumstances promote inflammation
Insulin resistance, high testosterone levels and clogged pores trigger an immune response. And because of this, your body initiates inflammation to resolve the issue. When your immune system can’t resolve the problems, you might begin to experience chronic inflammation.
4. Inflammation worsens acne severity and pain
The chronic inflammation doesn’t just affect one area, but spreads across your whole body. Inflammation in follicles leads to swelling, redness, tenderness, and cystic acne.
5. Chronic inflammation activates the stress response, raising cortisol levels
Persistent low-grade inflammation raises cortisol levels (stress hormones). Over time, this constant cortisol release can disrupt normal hormone balance and keep the body in a “fight or flight” mode.
When your body is constantly having to deal with inflammation, instead of just occasionally like its supposed to, it can cause a whole chain reaction of other issues throughout the body.
6. High cortisol increases oil production and slows skin repair
Cortisol stimulates oil production, too. That means more oil to block hair follicles and cause problems. It also slows skin repair by reducing collagen and slowing cell turnover, allowing dead skin cells to accumulate with the oil and clogged pores.
It’s important to say at this point, though, that cortisol isn’t entirely bad. Cortisol is a normal, natural and desired part of everyday living for times like waking up in the morning and during exercise. It only begins to be problematic when it’s elevated nearly all the time, which is not its intended status.
7. Elevated cortisol worsens insulin resistance
High stress levels and a constant “fight or flight” mode signal your body to conserve energy. This makes your body store more glucose, increasing insulin resistance.
This is also why a good sleep routine can help your gym goals, because better quality sleep can reduce cortisol levels overall and allow you to lose fat more easily (if that’s your goal).
8. The cycle repeats
The cycle then repeats: worsened insulin resistance boosts androgen production, leaving women with PCOS trapped in persistent, difficult-to-treat hormonal acne.
Does acne from PCOS go away?
Without getting to the root issue of PCOS acne, it won’t go away. No topical treatments or seasonal changes will clear up skin entirely.

But can PCOS acne go away with strategic lifestyle changes that address insulin resistance, hormonal imbalance, and inflammation? I personally think so.
Here are some things you can do to balance your body and clear up PCOS acne:
- Eat a balanced, anti-inflammatory diet
- Cut back on refined carbs overall
- Reduce your caffeine intake (I also talk about caffeine in this post). A morning coffee can be fine, but avoid having several throughout the day
- Stay hydrated
- Gently exercise (swimming, walking, pilates, weight lifting etc.)
- Get 7-10 hours of great sleep
- Practice stress-management (always easy to say but hard to do, I know!)
- Talk to your GP about supplements (inositol, zinc, and omega-3)
- Also talk to your GP about hormonal oral contraceptives
- I find retinoids and azelaic acid super helpful, but without other lifestyle changes the PCOS acne may not fully resolve
What is regular acne?
Regular acne, also called acne vulgaris, is mainly caused by bacteria, oil production and genetics. They are relatively similar conditions and there is often overlap, therefore it can be helpful to try out some of the strategies for PCOS acne to see if they help you.

It typically appears as whiteheads, blackheads, and sometimes inflamed bumps. Breakouts most often occur in the T-zone (forehead, nose, and chin) but can also appear on the cheeks, back, chest, and shoulders.
The way your acne presents can often vary depending on what is causing it, for example:
- Some teenagers start to get blackheads as puberty causes them to produce more oil and they don’t yet have a skincare routine. In this case, a skincare routine can often solve the entire problem.
- A woman in her mid 20s may randomly start to get hormonal acne because her situation changes a lot: maybe she’s in a stressful relationship and/or tries a new form of contraception that doesn’t agree with her.
- A woman in her 30s might suddenly have a lot of clogged pores because of a new product she’s using, but because she has always had clear skin she doesn’t suspect the new product. Her clogged pores can even become inflamed and so she sees a doctor for acne medication, even though it’s literally just the product!
What is the difference between hormonal acne and regular acne?
Cause
The root cause of each type of acne is different. Acne from PCOS, a hormone disorder, obviously comes from internal hormone imbalances. Regular acne can comes from dirt, debris, and bacteria – external sources. Essentially, one is internal, while the other is external. It can also be a mixture of both as acne is notoriously multi factorial.

This isn’t to say that someone with hormonal acne can’t also experience non-hormonal (regular) acne at the same time, and vice versa. Lots of people have a mixture of causes for the breakouts they’re experiencing such as:
- Genetics mean they are more prone to acne generally
- Their hormones are not as optimal as they could be
- One of their skincare products is not agreeing with them
- Perhaps their diet is low in fibre and protein which is causing them minor insulin resistance
- Maybe they tried a new supplement that is also breaking them out
Appearance
Hormonal acne shows up as deep, inflamed pimples. These breakouts are usually pretty painful, and they can even turn into cystic acne.
Regular acne isn’t usually painful. The pimples are small, superficial bumps, like whiteheads and flesh-colored bumps (closed comedones), as well as blackheads (open comedones).
Location
The U-pattern acne is on the jawline, chin, and lower cheeks. This is the shape of hormonal acne.

Regular acne, on the other hand, triggers breakouts in the T-zone. This is the forehead, nose, and upper cheeks. But as always, you can have both.
Duration
Since the causes of the acne are more circumstantial, regular acne usually resolves pretty quickly. This is especially true with proper skincare.
Hormonal acne lingers without much relief until the root issues are addressed. Most of the time, breakouts from hormonal changes won’t resolve themselves like regular acne does.
Treatment
Since the core issues of the acne types are somewhat different, they may require different treatment approaches.

For regular acne, ensure you have a strategic skincare routine for acne-prone skin. This will involve products with benzoyl peroxide that kill acne-causing bacteria and a topical retinoid, which helps keep pores clear.
Hormonal acne treatment is the above plus some lifestyle changes I listed about. A balanced diet, stress management, and great sleep go a long way.
However, even with hormonal acne, you want an intentional skincare routine. This can include double-cleansing, products with non-pore clogging ingredients, retinoids, and a lightweight moisturiser.
For more, read my guide on how to treat PCOS acne.
For more immediate relief, you may want to see a dermatologist about medication that could help: Spironolactone, birth control, accutane or WinLevi for example.
Hormonal acne and regular acne can both be treated, but require different approaches
Understanding the type of acne you have is key to effective treatment. Regular acne responds well to targeted skincare.
Hormonal acne requires addressing internal factors like hormones, insulin resistance, and inflammation. Treating each appropriately increases your chances of clearer, healthier skin.
If you liked this post, you might find these helpful, too: